Surgery
Making The Decision To Have Surgery
Surgery is the best option for people whose cancer can be safely and effectively removed. This usually means that the tumor hasn't grown into any of the major blood vessels located near the pancreas or spread to the liver, abdominal cavity or lungs.
Because pancreatic cancer is relatively silent in its early stages, less than 20% of all pancreatic cancer patients are eligible for surgery where the tumor is surgically removed (resected). Although improvements in diagnosis, staging, surgical techniques and postoperative care have led to much better outcomes after surgery, pancreatic resection is a demanding operation.
Types of Surgery
Most curative surgery is designed to treat cancers at the head of the pancreas, which is near the bile duct. Some of these cancers are found early enough because they block the bile duct and cause jaundice. Surgeries for other parts of the pancreas are only done when the doctor believes that he or she can completely remove the cancer.
Whipple Procedure
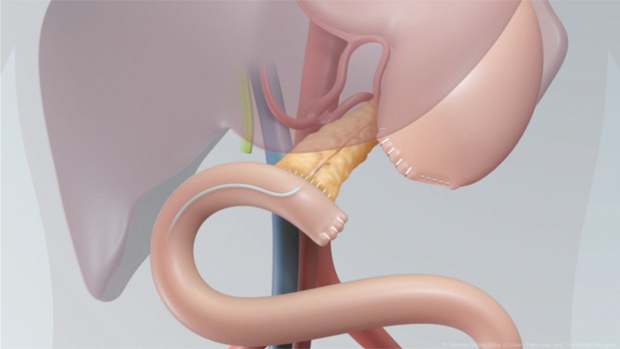
The Whipple Procedure, or pancreaticoduodenectomy, is the most commonly performed surgery to remove tumors in the pancreas. In a standard Whipple procedure, the surgeon removes the head of the pancreas, the gallbladder, part of the duodenum which is the uppermost portion of the small intestine, a small portion of the stomach called the pylorus, and the lymph nodes near the head of the pancreas. The surgeon then reconnects the remaining pancreas and digestive organs so that pancreatic digestive enzymes, bile, and stomach contents will flow into the small intestine during digestion. Surgery usually lasts between 6-10 hours.
Recent studies from Johns Hopkins and Memorial Sloan Kettering, major cancer centres in the United States, have shown that outcome from surgery for a Whipple operation is dependent on the experience of the hospital and the surgeon performing the surgical operation. In hospitals that perform a high volume of these procedures, the death rate from the Whipple operation is now less than 5%. In hospitals that infrequently perform the Whipple Procedure, complications from the surgery are often greater than 15 to 20%. Pancreatic Cancer Canada recommends that the Whipple operation be performed in a center that is experienced and does a high volume of these complex surgical procedures to ensure the best outcome.
The
Toronto Video Atlas of Liver, Pancreas and Transplant Surgery is a team of
multimedia developers and staff surgeons at the Toronto General
Hospital led by Dr. Paul Greig and Dr. Ian McGilvray,
who are providing an online library of surgical training videos that is freely
available to surgical trainees worldwide The following video utilizes 3D computer animation interspersed
between, or overlaid on, the surgical footage to clarify anatomical or
surgical aspects of the procedure. The following is a link to see this educational video:
Total Pancreatectomy
A total pancreatectomy involves the removal of the entire pancreas, as well as the spleen, gallbladder, common bile duct, and portions of the small intestine and stomach. By removing the pancreas, the chance of removing the entire tumor is increased. Unfortunately, a total pancreatectomy leaves the patient unable to produce pancreatic enzymes for digestion and insulin for controlling blood glucose level. The patient will be required to take supplemental enzymes and insulin for the remainder of his or her life.
Distal pancreatectomy
The bottom half of the pancreas is removed by a surgical procedure. The most frequent reason for performing a distal pancreatectomy is the presence of a tumor in the body or tail of the pancreas.
Potential Complications
- Pancreatic fistula or leakage of the pancreatic juice - In almost all patients who develop this complication after the surgery, the leakage heals on its own
- Paralysis of the stomach - It may take 4 to 6 weeks for the stomach to adapt to the changes after the surgery to function normally
- Mal-absorption: The pancreas produces enzymes required for digestion of food. In some patients removal of part of the pancreas during the Whipple operation can lead to a diminished production of these enzymes. Patients complain of bulky diarrhea type of stool that is very oily. Long-term treatment with oral pancreatic enzyme supplementation usually provides relief from this problem.
- Alteration in diet: After the Whipple operation it is generally recommended that the patients eat smaller meals and snack between meals to allow better absorption of the food and to minimize symptoms of feeling of being bloated or getting too full.
- Loss of weight: It is common for patients to lose up to 5 to 10% of their body weight compared to their weight prior to their illness. The weight loss usually stabilizes very rapidly and most patients after a small amount of initial weight loss are able to maintain their weight and do well.
Palliative Surgery
If doctors cannot perform a successful surgery because the cancer has spread outside the pancreas, pallative surgery is sometimes recommended to ease symptoms. In particular, uncomfortable symptoms such as jaundice, itching, nausea and bowel problems are caused by the cancer blocking the bile duct.
Stent
Having a small plastic tube (called a stent) fitted inside the duct helps to open up the bile duct and help to improve symptoms.
Biliary Bypass
Another way doctors can relieve the blockage to the bile duct is to cut the duct just above the blockage and rejoin it to the intestine. After the surgery, bile will bypass all or part of your bile duct and drain into the intestine.
Sources
www.surgery.usc.edu
www.mayoclinic.org