|
Palliative Care Palliative care or therapy is used to ease symptoms and manage pain regardless of the stage of the disease or the need for other therapies. The goal of palliative care is to improve quality of life not just in the body, but in the mind and spirit. While palliative therapies are clearly appropriate at the very advanced stages of the disease, they are also helpful when given in tandem with other cancer treatments still working to fight the disease. The focus of Palliative Care is neither to hasten nor postpone death. It provides relief from pain and other distressing symptoms and integrates the psychological and spiritual aspects of care. Furthermore, it offers a support system to help relatives and friends cope during the patient's illness and bereavement. Dealing with issues related to death and dying is a very difficult topic to broach. There is often the fear that if a patient is referred to palliative care they (or their doctors) are "giving up". This is a very one-dimensional approach to the services that can be offered. A Canadian palliative care leader, Dr. Larry Librach's vision, leadership and passion in advancing the field of palliative care is a true legacy that will live on and continue to benefit many Canadians to come. On May 23, 2013 Larry made one of his last contributions to this field with a candid video interview about his own personal experience facing a life-threatening illness, pancreatic cancer. Please take a moment to listen to this powerful and very informative piece.
What Are My Rights As A Patient?As a person facing a terminal diagnosis, I have the right to:
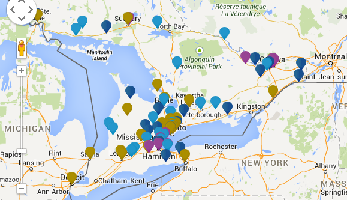
Inpatient Hospice Palliative Care Directory for residents of OntarioAlthough some people hope to remain at home for the duration of their illness, many people find that admission to an inpatient setting can also be helpful. The inpatient care settings in the directory below include palliative care units, residential hospices and dedicated palliative care beds within local hospitals. Inpatient hospice palliative care support includes 24 hour care, specialist pain and symptom management and psychosocial support for patients and families. UHN has provided a quick link with information and locations of inpatient hospice palliative care centres across Ontario. Click here to connect to their site which includes the map below provides access to a directory which includes more information about inpatient hospice palliative care settings across Ontario.
Resources |